
This is an interesting study that warrants validation in an unrelated cohort. Most accurate was a scale comprised of hemorrhage presentation, diffuseness, deep venous drainage, and the distance of lesion-to-eloquence with an area under the curve of 0.82. Several grading systems including the classic Spetzler-Martin scale were compared for accuracy in predicting mRS change. The lesion-to-eloquence distance was graded as 3, 2 and 1 for distances 10 mm. Shorter lesion-to-eloquence distance was associated with worse mRS. Good outcome was achieved in 94.5% of patients. Good outcome was considered a mRS of 0-2 at last follow-up. Mean duration of follow-up was 14.2 months. In 6% of patients, preoperative embolization or radiosurgery was performed. The group later used both LFPs and high gamma (70200 Hz) from the hand motor cortex to decode the time course of individual finger flexion activity. Two raters, blinded to the patient’s functional outcome as assessed by mRS, measured the lesion-to-eloquence distance from the nidus to the nearest functional eloquent cortex or eloquent fiber tract with consensus. KEY WORDS: Awake craniotomy, Cortical mapping, Eloquent cortex, Neurological.

Diagnose concussions and traumatic brain injuries (TBIs), which cannot be diagnosed with MRI. tive deficits, likely indicating close proximity of functional cortex to tumor.
The distance from the nidus to eloquence (eloquent cortex and fiber tracts) was measured. The eloquent cortex refers to areas of the brain that, if removed, would result in the loss of motor skills, sensory processing, linguistic ability, or paralysis.
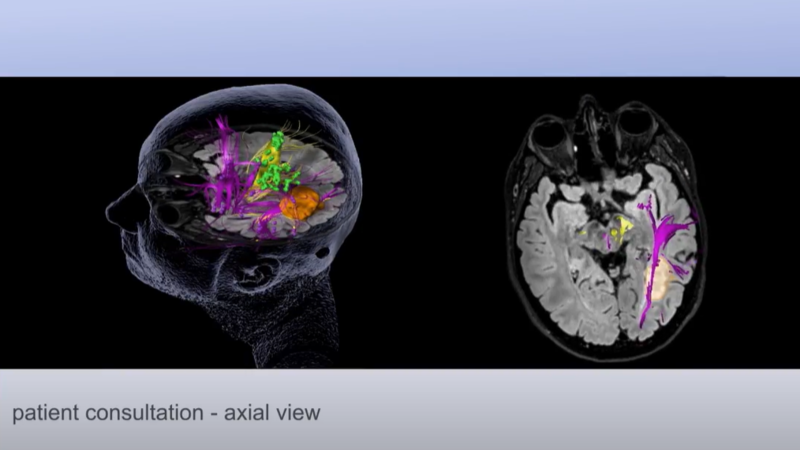
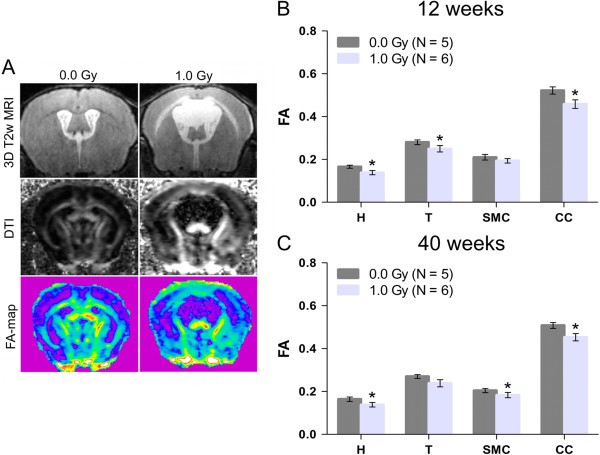
In a study published ahead-of-print this week in the Journal of Neurosurgery, 201 consecutive patients with brain AVMs that underwent preoperative functional MRI and diffusion-tensor imaging followed by microsurgical resection were assessed. Eloquence is one of the most critical features surrounding the natural history and management of brain arteriovenous malformations (AVMs).


 0 kommentar(er)
0 kommentar(er)
